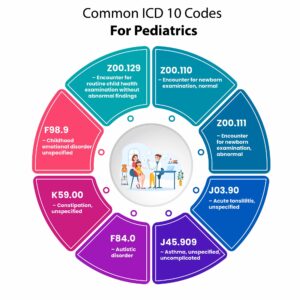
Common ICD 10 Codes For Pediatrics
In the realm of weight management, accurate medical coding is pivotal for effective patient care, streamlined billing processes, and appropriate reimbursement. Weight loss clinics, in particular, must navigate the complexities of the International Classification of Diseases, Tenth Revision (ICD-10), to document diagnoses and procedures accurately. This comprehensive guide delves into the most pertinent and common ICD-10 codes related to weight loss clinic, providing healthcare professionals with the knowledge to enhance their coding practices. Additionally, we’ll explore how DocVilla’s Electronic Health Record (EHR) and Electronic Medical Record (EMR) software can facilitate seamless coding integration, thereby optimizing clinical workflows. … Read More


















